A liver transplant is an operation that replaces a patient's diseased liver with a whole or partial healthy liver from another person. It is the second most commonly transplanted major organ, after the kidney.
Who Needs a Liver transplant ?
1. Acute Liver Failure
Acute liver failure, also known as fulminant hepatic failure, occurs when a previously healthy liver suffers massive injury resulting in clinical signs and symptoms of liver insufficiency. Any number of things can lead to acute liver failure but the most common causes are acetaminophen, ingestion of a toxin such as poisonous mushrooms, or an idiosyncratic drug reaction.
2. Chronic Liver Failure
The liver has a remarkable ability to repair itself in response to injury. Nevertheless, repeated injury and repair, typically over many years and even decades, scars the liver permanently. The end stage of scarring is termed cirrhosis and corresponds to the point where the liver can no longer repair itself. Once a person has cirrhosis, he or she may begin to show signs of inadequate liver function. This is termed "decompensated liver disease." Although medications can decrease the symptoms caused by the liver failure, liver transplantation represents the only permanent cure.
Related Article :
- Cirrhosis of Liver
- Causes of Hepatomegaly
- 7 Tips for Better Digestive Health
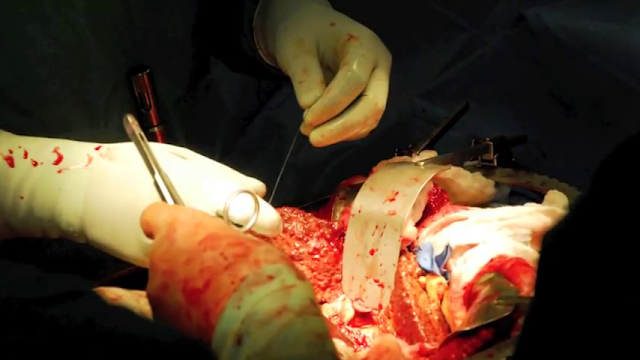
The Liver Transplant Operation
For someone undergoing liver transplantation, the sequence of events in the operating room is as follows :
1. Incision
2. Evaluation of the abdomen for abnormalities that would preclude liver transplantation (for example: undiagnosed infection or malignancy)
3. Mobilization of the native liver (dissection of the liver attachments to the abdominal cavity)
4. Isolation of important structures (the inferior vena cava above, behind, and below the liver; the portal vein; the common bile duct; the hepatic artery)
5. Transection of the above mentioned structures and removal of the native, diseased liver.
6. Sewing in the new liver: First, venous blood flow is re-established by connecting the donor's and the recipient's inferior vena cava and portal veins. Next, arterial flow is re-established by sewing the donor's and recipient's hepatic arteries. Finally, biliary drainage is achieved by sewing the donor's and recipient's common bile ducts.
7. Ensuring adequate control of bleeding
8. Closure of the incision
References
1. Transplant Surgery
http://transplant.surgery.ucsf.edu/conditions--procedures/liver-transplantation.aspx
2. Liver Transplant Surgery by Dr. Mark Ghobrial
Related Article :
- Cirrhosis of Liver
- Causes of Hepatomegaly
- 7 Tips for Better Digestive Health
Who Needs a Liver transplant ?
1. Acute Liver Failure
Acute liver failure, also known as fulminant hepatic failure, occurs when a previously healthy liver suffers massive injury resulting in clinical signs and symptoms of liver insufficiency. Any number of things can lead to acute liver failure but the most common causes are acetaminophen, ingestion of a toxin such as poisonous mushrooms, or an idiosyncratic drug reaction.
2. Chronic Liver Failure
The liver has a remarkable ability to repair itself in response to injury. Nevertheless, repeated injury and repair, typically over many years and even decades, scars the liver permanently. The end stage of scarring is termed cirrhosis and corresponds to the point where the liver can no longer repair itself. Once a person has cirrhosis, he or she may begin to show signs of inadequate liver function. This is termed "decompensated liver disease." Although medications can decrease the symptoms caused by the liver failure, liver transplantation represents the only permanent cure.
Related Article :
- Cirrhosis of Liver
- Causes of Hepatomegaly
- 7 Tips for Better Digestive Health
 |
| Anatomy Of Liver |
The Liver Transplant Operation
For someone undergoing liver transplantation, the sequence of events in the operating room is as follows :
1. Incision
2. Evaluation of the abdomen for abnormalities that would preclude liver transplantation (for example: undiagnosed infection or malignancy)
3. Mobilization of the native liver (dissection of the liver attachments to the abdominal cavity)
4. Isolation of important structures (the inferior vena cava above, behind, and below the liver; the portal vein; the common bile duct; the hepatic artery)
5. Transection of the above mentioned structures and removal of the native, diseased liver.
6. Sewing in the new liver: First, venous blood flow is re-established by connecting the donor's and the recipient's inferior vena cava and portal veins. Next, arterial flow is re-established by sewing the donor's and recipient's hepatic arteries. Finally, biliary drainage is achieved by sewing the donor's and recipient's common bile ducts.
7. Ensuring adequate control of bleeding
8. Closure of the incision
References
1. Transplant Surgery
http://transplant.surgery.ucsf.edu/conditions--procedures/liver-transplantation.aspx
2. Liver Transplant Surgery by Dr. Mark Ghobrial
Related Article :
- Cirrhosis of Liver
- Causes of Hepatomegaly
- 7 Tips for Better Digestive Health













Post a Comment